New AUA Guidelines for Early Stage Testicular Cancer
I’m pleased to see that the new American Urological Association Guidelines on the Diagnosis and Treatment of Early Stage Testicular Cancer have finally been published, and it was a great honor to be a small part of this!
I’m pleased to see that the new American Urological Association Guidelines on the Diagnosis and Treatment of Early Stage Testicular Cancer have finally been published, and it was a great honor to be a small part of this!
Link: https://www.auanet.org/guidelines/testicular-cancer-guideline
Unlike the National Comprehensive Cancer Network NCCN Guidelines for Testicular Cancer which covers all stages and treatments, this new AUA guideline is focused specifically on earlier stage patients up to and including Stage IIB.
As stated in its purpose, “A priority for those patients with low-stage disease is limiting the burden of therapy and treatment-related toxicity without compromising cancer control. Thus, surveillance has assumed an increasing role among those with cancer clinically confined to the testis. Likewise, paradigms for management have undergone substantial changes in recent years as evidence regarding risk stratification, recurrence, survival, and treatment-related toxicity has emerged.”
And with that, these AUA guidelines for earlier stage Testicular Cancer patients were born, at the Johns Hopkins University Evidence-based Practice Center in Baltimore, MD.
Why Early Stage Specific Guidelines Matter
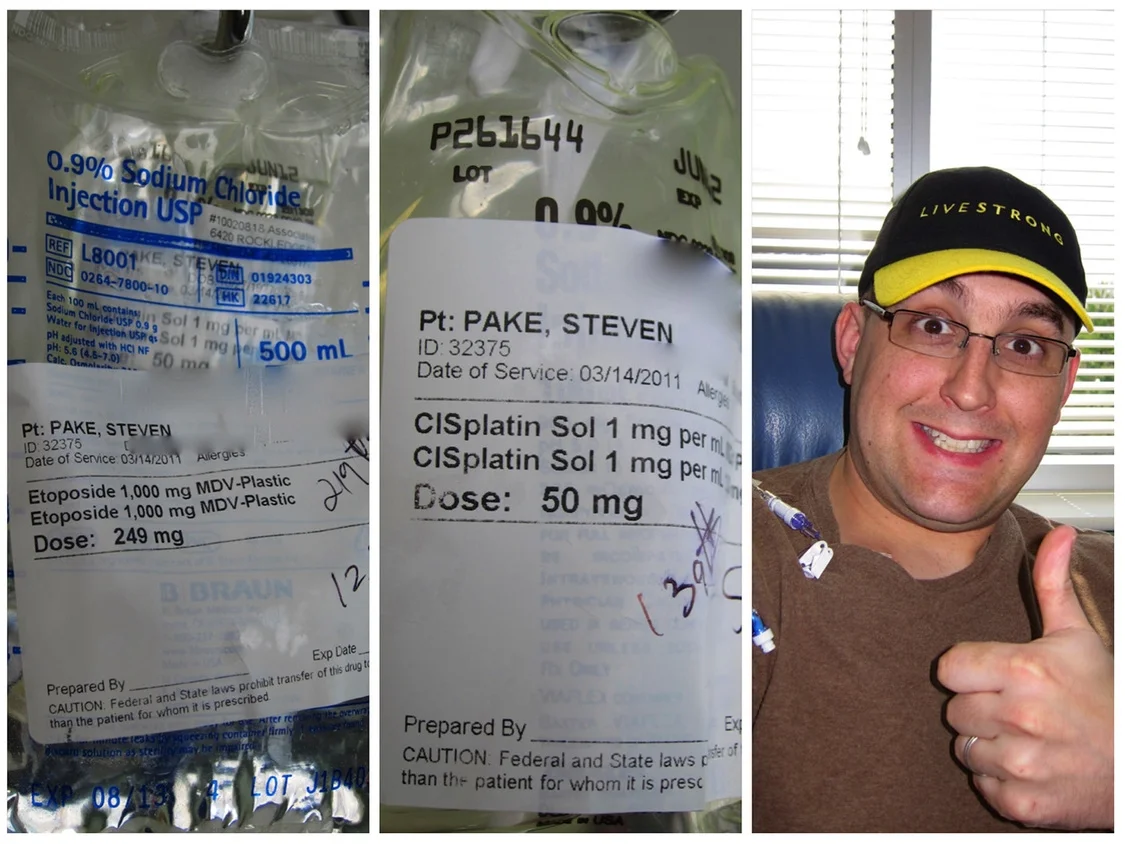
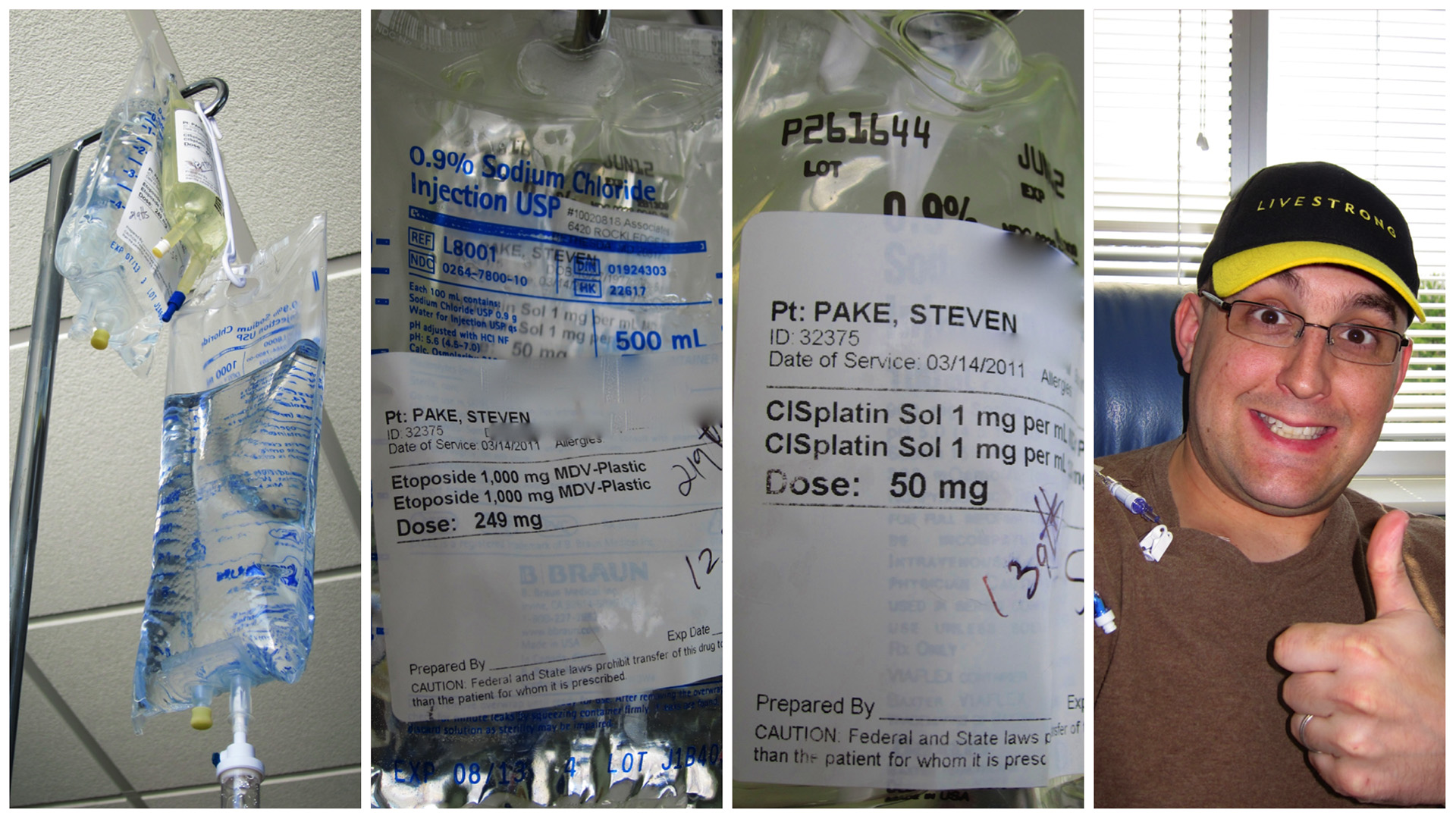
As a Stage IIB patient diagnosed back in 2011, I ended up having to go through the wringer for treatments, and suffered quite a bit in the aftermath from chemotherapy induced peripheral neuropathy pain (CIPN), and from chronic fatigue and pain issues, among other things. I had nightmares about everything I had been through for years, and suffered from PTSD symptoms at times, and other mental health issues as well. To this day, I still experience regular physical - but tolerable - pain that can be attributed to my cancer treatments 8 years ago, which is why I’ve always tried my best to help educate the testicular cancer community about the potential ramifications of treatments, and that the focus shouldn’t just be on getting cured, but to also minimize the potential burden of treatments. These chemotherapy drugs are a miracle and why I’m still here to write this, but they’re no joke as far as potential long-term effects to our bodies and quality of life. We only have one body to make it through our entire lives, and testicular cancer tends to strike younger men who will have to live with whatever permanent effects there might be from treatments for much longer than the typical cancer patient who is diagnosed much later in life. This is why it’s so important to focus not just on achieving a cure, but doing so with as little collateral damage as possible “without compromising cancer control.”
As I wrote in my blog about the RPLND surgery, if I had done that surgery first as the primary treatment, and then followed up with chemotherapy afterwards, I likely wouldn’t have suffered a loss of fertility from the RPLND surgery, because it’s a far easier surgery to do prior to any chemotherapy (which makes preserving the ejaculatory nerves much easier), but I also likely only would have needed half of the chemotherapy and probably wouldn’t have suffered nearly as much of the neuropathy pain and chronic fatigue issues that I did for years. These things have all had non-trivial impacts on my quality of life after cancer in addition to my fertility, and all of that matters to the earlier stage testicular cancer patients who will have numerous decades of life still in front of them in the vast majority of cases.
Presentations by both Dr. Phil Pierorazio and Dr. Lawrence Einhorn at the first Testicular Cancer Summit back in 2017, gave me hope that things were headed in the right directions as far as managing testicular cancer treatments and the patient population. Both “Dr P” and “Dr E” and other amazing doctors present proved through both their words and the compassion the displayed, that they truly understood the lives of their patients and their challenges after cancer. These AUA guidelines for earlier stage testicular cancer patients are a perfect embodiment of their visions laid out for the future of testicular cancer management.
Hello there! :)
The AUA Testicular Cancer guidelines were authored and then reviewed by dozens of doctors and testicular cancer experts both internally and externally to the AUA. It was a great honor to be one of just three non-MD reviewers of these guidelines, along with my friend and fellow survivor Mike Craycraft from the Testicular Cancer Society, and Sam Gledhill, who runs the Global Testicular Cancer Programs for Movember Foundation. Admittedly, much of what’s in these guidelines were well above my pay grade, but serving as a non-medical external reviewer was an invaluable opportunity to provide patient and survivor community feedback on various issues to the world’s foremost experts on testicular cancer, to which I took full advantage. Just having my name on the same page as Dr. Lawrence Einhorn, the father of the cure for testicular cancer, is a huge honor, and a nice way to cap off my years of advocacy work in the testicular cancer community.
The AUA early stage Testicular Cancer guidelines are written more for medical professionals and are not exactly patient friendly to read, but there’s a wealth of information present in them. For a more patient friendly guide to testicular cancer, check out the National Cancer institute’s guide to testicular cancer (linked below), where they also have a more advanced medical professional version linked as well. The latest NCCN Guidelines for Testicular Cancer are another must read if you’re really serious about understanding testicular cancer treatment paths through all stages, and are available online for free after registration at the NCCN website.
Links
AUA Early Stage Testicular Cancer Guidelines (PDF)
NCCN Testicular Cancer Guidelines
National Cancer Institute - Testicular Cancer Patient Version (Medical Professional Version)
I’m not very active on social media and support groups these days due mostly to a lack of time, but am always happy to talk to anyone about anything related to testicular cancer through my contact link, which will go straight to my phone. Whether you’ve just been diagnosed with testicular cancer and are trying to understand different treatment options, or you’re struggling with life after cancer, I’m always available for the testicular cancer community, even if I haven’t been very visible as of late. Definitely drop me a line! I’m always here.
Thanks again to the AUA Team for the opportunity to serve as an external reviewer of these guidelines.
Best,
Steve Pake
April is Testicular Cancer Awareness Month
April is testicular cancer awareness month, and as a 9 year survivor of this disease, I can tell you a few things about testicular cancer.The first is that contrary to what people might expect, testicular cancer is actually the #1 form of cancer in men ages 15-44 internationally, yet almost no one talks about the disease. It’s sad and frustrating that 20 years after the founding of a very famous organization in yellow by a now very infamous testicular cancer survivor, that we still have to struggle so hard for any sort of public awareness about this disease. Testicular cancer in young men is about as common as breast cancer is in young women, yet no one ever talks about testicular cancer! In the U.S. alone, someone is diagnosed with testicular cancer every hour, and someone dies of this disease every day.
April is Testicular Cancer Awareness Month, and as a 9 year survivor of this disease, I can tell you a few things about testicular cancer.
The first is that contrary to what people might expect, testicular cancer is actually the #1 form of cancer in men ages 15-44 internationally, yet almost no one talks about the disease. It’s sad and frustrating that 20 years after the founding of a very famous organization in yellow by a now very infamous testicular cancer survivor, that we still have to struggle so hard for any sort of public awareness about this disease. Testicular cancer in young men is about as common as breast cancer is in young women, yet no one ever talks about testicular cancer! In the U.S. alone, someone is diagnosed with testicular cancer every hour, and someone dies of this disease every day.
With an overall cure rate of over 90%, testicular cancer is a highly curable cancer, but it should never be considered an easy or a “good” cancer. Testicular cancer tends to be a pretty fast growing and aggressive form of cancer, and must be hit equally aggressively in order to get that cure. Orchiectomy alone, removal of the stricken testicle, can be enough to cure many Stage I patients, but the primary chemotherapy protocols and surgeries that are commonly used to treat people with metastatic disease are pretty rough, and can leave many additional physical and mental marks on people.
Regardless of the stage of the disease at diagnosis, testicular cancer is not an easy cancer to get through simply because of the younger men that it tends to strike. My 33 year-old self was unaccustomed to ever having anything more than the flu, and still believed that I was invincible and going to live forever. This loss of innocence and suddenly feeling so vulnerable at the prime of my life shattered my confidence. Mental health issues such as anxiety and depression are common, and posttraumatic stress to varying degrees is certainly not unheard of, either. Another thing that young men aren’t typically accustomed to doing, is asking for help when they need it. The rarity of young adult cancers can tend to leave survivors feeling very isolated and lost, which is why finding support from the young adult cancer community is essential. Regardless of gender or cancer type, young adults tend to face so many of the same inner struggles after a cancer fight. No one needs to fight alone.
There are a few risk factors for testicular cancer that include an undescended testicle, a family history of the disease, and being Caucasian, but most testicular cancer diagnoses simply come down to bad luck. Signs and symptoms include a painless lump or any change in size or any irregularity in the testicles. Pain or discomfort in the testicles, or any pressure sensitivity is certainly a potential sign, along with a dull ache or a sense of pressure in the lower back, abdomen, or groin. More advanced signs include significant weight loss, back or chest pain and coughing or difficulty breathing, and enlarged lymph nodes in the abdomen or neck.
Because testicular cancer isn’t preventable, monthly testicular self-exams are recommended for all men, and boys starting at 13. There are some groups out there that say not to bother, given that testicular cancer is so curable at any stage. This is terrible advice. Don’t listen to it. Just because a cancer has a high overall cure rate, doesn’t mean you should ignore any signs or symptoms until you have very advanced stage disease. I was lucky in that I actually had pain in my testicle that clued me in that something wasn’t right, and a thorough self-exam found the solid mass. Not everybody does, and that painless lump can quickly turn into a very dangerous advanced stage cancer in just a matter of months. Poor risk testicular cancer has a 50/50 cure rate, no better than a coin toss! Why leave your life up to a coin toss?
Believe me when I say that if you’re going to develop testicular cancer, you’re much better off catching it an early stage rather than late, as you’ll avoid significant trauma to both mind and body if you’re able to avoid some of the harsh treatments and surgeries that are used to cure metastatic testicular cancer.
There’s nothing to lose with a regular feel down below, and it could save your life.
StevePake.com
Negotiating Surveillance and Long-Term Follow-up for Testicular Cancer
The National Comprehensive Cancer Network (NCCN) Guidelines for are the bible by which Testicular Cancer patients are treated and managed. The follow-up care recommendations within these guidelines only goes out to 5 years, and even within those 5 years, there's been some significant adjustments to the recommendations over time. It's entirely possible that if you were diagnosed with testicular cancer within the past few years, that you might be able to make some adjustments to your follow-up schedules in favor of fewer scans or appointments, but what do you do after that? It's up to you and can go on a case-by-case basis. Here are some answers.
The National Comprehensive Cancer Network (NCCN) Guidelines are the bible by which Testicular Cancer patients are treated and managed. The follow-up care recommendations within these guidelines only goes out to 5 years, and even within those 5 years, there's been some significant adjustments to the recommendations over time. It's entirely possible that if you were diagnosed with testicular cancer within the past few years, that you might be able to make some adjustments to your follow-up schedules in favor of fewer scans or appointments, but what do you do after that? It's up to you and can go on a case-by-case basis. Here are some answers.
Changes to NCCN Follow-Up Recommendations Within Years 1-5
The NCCN Guidelines are literally the most important guide for any cancer fighter or survivor to have, and the bible by which doctors should be treating their patients.
First off, there have been many, many changes to the NCCN follow-up recommendations since I was diagnosed with testicular cancer in 2011, and the latest testicular cancer guidelines (2-2017 as of this writing) states that "further study is required to define optimal follow-up durations." In other words, they just don't have the evidence to know what the best answer is here. What is too much and what's too little? Scan frequency has gone down quite a bit to minimize the risk of secondary malignancies from radiation exposure, especially from CT scans, but they don't have the evidence to know where the sweet spot is, thus making these follow-up schedules very much open to debate and negotiation. Yes, your follow-up schedules for testicular cancer are negotiable.
In my case, for Stage II non-seminoma good risk disease treated with both primary chemotherapy and the RPLND surgery, the changes to the follow-up recommendations have been significant. At the time of my diagnosis in 2011, the NCCN guidelines called for as many as 20 scans (chest x-rays) and follow-up appointments over 5 years. I was seen at Memorial Sloan Kettering Cancer Center (MSKCC) in New York who went above and beyond the guidelines, and I had a total of 27 chest x-rays over the years, with 18 of those coming in the first two years alone. Given I had the RPLND surgery, only one CT scan was needed 4 months post-op, and otherwise just chest x-rays for me.
As of 2017, how many scans are recommended by the NCCN guidelines for someone like me now?
SEVEN.
Just 7, with 8th and 9th scans in Years 3 and 4 being optional, and no scans at all in Year 5. Granted, I'd still need a total of about 16 office visits, but that's still a whole lot less stressful than twenty-freaking-seven. When I first saw how significantly the NCCN follow-up recommendations had changed and how many fewer scans they were recommending these days, I about fell out of my chair, and then needed to go sulk in a corner for awhile. This is really great news, as it shows that, yes, treatments for testicular cancer really are highly effective and completely curative most of the time, and that there really isn't a whole lot to be afraid of, despite the unavoidable and unimaginable amounts of worrying that it brings patients. Most people are just fine after treatments. Thanks to our collective piles of chest x-rays and CT scans that have never shown anything for most over the years, testicular cancer survivors will have far fewer scans to worry about after treatments today, and that's a very good thing.
Making Mid-Course Surveillance Schedule adjustments
A part of me regrets not questioning so many scans, especially now that not even a third of those scans are required today, but that's water under the bridge at this point. It wasn't easy, to put it mildly, but I got through them all. If you were diagnosed with testicular cancer a few years ago, there's a chance that you might still be on a more scan-heavy schedule. If so, you might be able to modernize your follow-up schedule after review with your doctors. Here's what you can do:
- Download the latest NCCN guidelines by registering for free at the NCCN website. Navigate to the Guidelines section, then to Cancer by Site, and then Testicular Cancer to get to them. Find the follow-up table that's relevant for your cancer about midway through the document based on type (seminoma or non-seminoma), and then stage, treatment path, and level of treatment received, and pay close attention to the super-scripted notes. Review what the current follow-up recommendations are now, against what you're actually doing. It might be quite different.
- Review With Your Doctor. With how many scans they've pulled from the follow-up schedules in recent years, chances are you might not need nearly as many now, or perhaps you could just do chest x-rays for scans and skip any further CT scans at this point, followed by the usual history and physical, and blood tumor marker checks? No more CT scans, wouldn't that be nice? If you look very closely in the guidelines you'll also see that scrotal ultrasounds are now mentioned as well. Sound like something worth doing? It was for me, and I'll get to that below.
- Do What's Best For You, with Your Doctor's Blessing. Whether you're at the point of cutting yourself free from oncology care if you so choose, or are making mid-course corrections between 1-5 years out, do what's right for you, so long as your doctors are on-board with your plan. There's both "scanxiety" from the follow-up appointments, but also anxiety from not having them. I don't know of a single person that actually enjoys getting CT scans done, but some might have more anxiety without them. Be true to yourself and your needs. If you're struggling, it can be worth it to make adjustments, and still meet the standards for care.
Of course, now that I've made it through 5 years and twenty-seven freaking scans, I have the moment of revelation that maybe I should have asked more questions than I did, but most of these scans were in the first two years, and before the NCCN started pulling back on the number of scans required. What's done is done, and I'm happy to have exited my 5 years of active surveillance.
How To Make Your Post 5 Year Follow-Up Plan
So, what to do after 5 years? Here's what I did.
You're the patient, you're the boss. You can do whatever you want to do after 5 years. If you feel like you're ready, you can opt to be formally discharged from oncology care, or if not, you can continue to be seen at whatever interval you're comfortable with. Your doctor will be more than happy to keep seeing you. It's up to you, and there's no right or wrong answer. The correct answer is whatever you're comfortable doing, with considerations for any specifics of your case, and that your doctors are on-board with.
For me, with good risk disease, primary chemotherapy and the RPLND which most people in my risk classification tend to skip, I just needed to be cut free. If I'd only had 7 to 9 scans and a dozen and change office visits over the years as opposed to 27 of them, maybe I'd still want annual follow-ups with my oncologist. Maybe I'd still want annual follow-ups had I skipped the RPLND, and I'm quite certain I'd still want them were I in a higher risk group. Instead, I've found myself totally and completely burned out emotionally from so many oncology office visits, and I just didn't want to have to keep going if there was no compelling reason to do so. I love my oncologist and he's a great guy, and my favorite oncology nurse (hello Trish!) has become a friend for life type with me, but I just needed to walk out of that office for once without another appointment scheduled. I really needed that like nothing else, otherwise everything would just keep perpetuating in my mind. I needed the closure of not having to go back, and so we developed a plan that supported that.
The first condition for my formal discharge from oncology care, both from my wife and from my oncologist, was the insistence that I have an annual physical exam done by my primary care every year. No problem there, and cancer survivors especially should have these done annually as it is. Next up, scans or no scans? For my stage of disease and level of treatments, one is more likely to see a false positive from a chest x-ray at this point than disease recurrence, and so I opted out of any more chest x-rays. I think 27 has been more than enough. Although my tumor markers (bHCG and AFP) had always been negative and resulting blood work not that useful, I elected to continue doing these. You're having blood work done at an annual physical anyways, so why not throw it in? Continuing with these tests are useful for catching a potential second primary testicular carcinoma that might have a slightly different signature, and that could be positive for these markers.
Testicular Ultrasounds. This is something that I'd highly recommend doing for every testicular cancer survivor out there at least annually. Testicular ultrasounds weren't in the NCCN guidelines when I was diagnosed with testicular cancer back in 2011 other than for initial workup, but they're included now for follow-up care as well, for obvious reasons. As with the above, testicular cancer survivors are at elevated risk for developing testicular cancer again on the other side versus the general population. If anything was ever going to catch this early, and give a heads-up that something is going on before there were symptoms or other signs, a testicular ultrasound is what could do it, and so this was a no-brainer thing to do.
Do a full hormone panel. It's not mentioned anywhere in NCCN, and not something that oncologists ever really pay much attention to, but get a full hormone panel done. Despite what doctors say about the other testicle "picking up the slack", there is literally no information out there to support that, and we survivors know very well that this isn't necessarily true. It's a given that we're far more likely to face hormonal issues as we age due to only having a single testicle. Almost nothing is known about male hormones, and we're pretty much on our own here. The more data points we have on ourselves, the easier it will be in the future to know what's going on, if and when hormonal issues do develop.
Why a full hormone panel and not just a testosterone level check? Some long-term testicular cancer survivors who are symptomatic of hypogonadism are finding not that their testosterone levels are too low, but rather that their estrogen levels are too high, and have had some success in being treated with estrogen inhibitors, rather than testosterone replacement therapies. Please note that this is all highly experimental reports from individuals within the testicular cancer community, and not from official studies, of which there are none to go on. The point is, just start collecting as much hormonal data about yourselves as you can now, as it will potentially be very useful later.
STICK WITH YOUR PLAN
Honor yourself, the doctors and nurses that helped you through your cancer treatments, and your family and friends that have been there for you as well, by sticking with whatever your agreed upon plan is. After the hell that so many of our bodies have been through fighting cancer, and the significant emotional investments made by so many supporting us, we owe it to ourselves to do everything we possibly can to maintain the best possible health for ourselves going forward. A big part of that is having an annual physical done, and should be a part of every cancer surveillance exit plan.
I'm happy to say that I just had my annual physical, and that it went very well. My cholesterol, HDL/LDL levels and ratio were all good, as was my blood pressure and fasting glucose levels. A few things that have been messed up since fighting cancer are still messed up, but stable. My creatinine levels have been 1.4-1.6 since cancer (normal was around 1.0 before), due to some damage to my left kidney sustained from chemotherapy, and then a complication from the RPLND surgery didn't help it out at all. My platelet levels also run low at around 100, which is due to some permanent bone marrow damage also due to chemotherapy. None of that has changed in years, and it's good to know that.
One thing in my CBC report has tracked a bit high, but that's always correlated with my weight, and I've vowed this year to finally lose every last "cancer pound" I'd ever gained. Before cancer, I was around 240-250 pounds, which was considered to be a good weight for me considering my significant height of 6'3", and my large frame. Because of how chemotherapy, steroids, and surgeries had all affected me while fighting cancer, I ballooned all the way up to 300 pounds as I exited MSKCC in New York after my RPLND surgery. Due to chronic post-cancer fatigue from chemotherapy induced peripheral neuropathy, I could never exercise hard enough in my first few years after cancer to burn that off. My weight has floated around 270 pounds for the past few years, but running helped me to get beyond my fatigue issues, and there's no excuse anymore.
I refuse to turn 40 later this year in anything other than the best shape of my life. When we Scorpios commit to something, we're either all-in 110% or don't bother, and so I'm all in with a gym membership and regular exercise, a strict diet and paleo foods, and all that. This will happen. Turning 40 will be the start of a new era and decade for me, and this baggage from cancer, including the residual flab on my sides, is not going to be a part of that.
At the time I walked out of my oncologist's office for hopefully the last time ever back in June of 2016 (knocking on wood), I wasn't able to really feel or appreciate that moment at the time due to so many other things going on in our lives. As I'm typing this now, over a half year later, I'm finally feeling that emotional release and tears of joy from this for the first time, and the relief of such an enormous burden in my life having been lifted.
I just couldn't accept having to keep seeing an oncologist every year for the rest of my life. I've finally made it. I know how quickly things can change, and am going to keep living my life exactly how I've learned to LIVE it after cancer, but this is done now.
I'm finally free, and I can't wait to see so many friends and connections I've made in the testicular cancer community finally reach this huge milestone, too.
StevePake.com
"Testicular Cancer Wasn't That Bad?"
I'm amused that the ink has hardly dried on my last blog titled "There Is No Easy Cancer," only to now see an article over at GQ titled, "I Had Testicular Cancer and It Wasn't That Bad." Oh my...
March 2011, sick as a dog after my first round of chemotherapy. Look, I still had eyebrows too!
I'm amused that the ink has hardly dried on my last blog titled "There Is No Easy Cancer," only to now see an article over at GQ titled, "I Had Testicular Cancer and It Wasn't That Bad." Oh my...
I applaud Jason Kessler, who wrote the story, for being open about his cancer experience, and that his treatments including the orchiectomy and BEPx3 chemotherapy weren't overly rough on him. It's actually encouraging for people to know that yes, you can and will get through this, except that the "end" of his story is getting a clear CT scan a month after his chemotherapy had ended. One of the biggest lessons that I've learned in nearly five years of having survived a Stage II testicular cancer very similar to Mr. Kessler's, is that the end of our cancer fights are really just the beginning of our journeys. As I look back on these five years, it's so clear that fighting my cancer was the easy part - everything that came after was so much harder.
Cancer survivorship is a rude awakening for so many of us. As I wrote in "Cancer Survivorship - The Fight After the Fight," there were so many new things that I had to deal with for the first time after cancer, that I was simply unprepared to even know how to handle. I developed secondary health and severe pain issues from the harsh treatments my body had to endure. There was so much anxiety about countless follow-up scans, I've suffered from depression and post-traumatic stress, issues with testosterone levels that were swinging back and forth, terrible muscle fatigue issues, and on and on. I too had almost thought that maybe what I went through wasn't so bad at one point a year after my cancer fight, but I unknowingly had kept all of my fears and emotions about everything bottled up inside of me. It wasn't until nearly two years later that the dam had burst, and all of this finally started processing. And when it did, it hit me like a load of bricks.
All of the uncertainty, and my life constantly being up in the air every other month with the latest round of scans and blood work, broke me as a person. I couldn't live like that anymore, and had to learn how to live my life all over again. This doesn't happen overnight. It's only now that I'm about to reach nearly five years out since cancer entered my life, that I finally feel like my life really has moved on after cancer. For many, cancer survivorship isn't an easy ride even with a so-called "easy" cancer like testicular cancer. There is no easy cancer.
A word of caution is also needed about medical marijuana usage, as marijuana use can also elevate the HCG testicular cancer marker in men. I've run across a few people over the years in total freak out mode that their HCG levels came back elevated on surveillance blood work. They had been in tears thinking their cancers had returned, unaware of the possibility of this marker being elevated due to marijuana usage. It's not a good situation to be in at all. I'm actually a proponent of legalized and/or medical use for marijuana. There's something to be said about medical marijuana usage and its ability to relieve certain side-effects both during and after fighting cancer, but one needs to be aware of this possibility in the context of a discussion about testicular cancer!
There's also no guarantee that one will feel any pain if they have testicular cancer, either. You're not necessarily just going to know! You're lucky if you do, as both I and Mr. Kessler were, because it means you can catch it at an earlier stage. Testicular cancer can be a silent killer, overrunning your entire body with no symptoms at all for months, until you suddenly find yourself in the ER one day coughing up blood, or with other bizarre symptoms due to organs starting to shut down! They don't even wait to do the orchiectomy or pathology in many of these cases. They start you on chemotherapy that day, because you might not have another day left! Plenty of advanced stage testicular cancer patients never had any pain to clue them off, and this is why awareness of the disease, and testicular self-exams are so important. Pain in a testicle isn't a sure thing, but you might be able to detect an abnormal lump on your own. There are also testicular cancer cases that are extragonadal, and don't even start in the testicles at all. It's not nearly as simple as Mr. Kessler made things out to be.
I genuinely pray that Mr. Kessler has a smooth and easy ride through his survivorship years. God bless him if he does, but he would be in a slim and incredibly fortunate minority. I know quite a few testicular cancer survivors, and so many of us are blindsided by the challenges we face in our lives after cancer. I asked a group of survivor friends for feedback on this article, and very few thought that Kessler's experience was representative of what a typical testicular cancer patient goes through, and a few thought that he was in denial about some things. One caregiver friend whose son had testicular cancer, was in tears about how dismissive the article felt in the face of what she, her son, and other friends had all been through fighting this disease.
Testicular cancer continues to be a real disease that kills real people every single day. Many have lost loved ones, husbands, fathers, and sons. For these people, seeing an article like this around the holidays while trying to get on without, is painful to say the least. For the majority of us that do survive, the high cure rates tend to be of little comfort when you're the one in the hot seat with strange pains in your body, and you're worried to death about your next set of surveillance scans. The challenges of life after cancer are not to be underestimated. Should Mr. Kessler find himself in a situation after cancer that he's completely unprepared to handle, he should know that there's a sizable community of fellow young adult cancer survivors waiting in the wings to support him through whatever he needs.
StevePake.com
There Is No Easy Cancer
On at least two occasions when I've mentioned my cancer story to new friends or acquaintances that hadn't known, I've received comments that were just short of dismissive that testicular cancer is an "easy cancer", alluding to the high cure rate. I'll be honest in saying that I haven't been offended by such comments, because I know that short of having been there in some way themselves, it's simply impossible for people to truly know what a cancer diagnosis feels like, nor all that one entails.
This is what I looked like after 5 months of hell fighting cancer and getting the massive RPLND surgery. I was all bald and bloated and disgusting feeling, having gained 30 pounds from the crazy ways in which the chemotherapy had affected my body. I had never been in more physical pain, nor more uncomfortable in my entire life, but believe it or not, this was the easy part of fighting cancer.
On at least two occasions when I've mentioned my cancer story to new friends or acquaintances that hadn't known, I've received comments that were just short of dismissive that testicular cancer is an "easy cancer", alluding to the high cure rate. I'll be honest in saying that I haven't been offended by such comments, because I know that short of having been there in some way themselves, it's simply impossible for people to truly know what a cancer diagnosis feels like, nor all that one entails.
Regardless of the type of cancer and early or late stage, the fact is, cancer turns your life upside down. Especially as young adults, we have so much of our lives left to live, and we wonder if we'll ever be able to live our hopes and dreams at all. Cancer forever casts a dark cloud over us, and it's a difficult adjustment to make when we're supposed to be brimming with optimism about our futures. There was nothing easy about the five months of toxic treatments and brutal surgeries that I had to endure, to get through my Stage II cancer. There was also nothing easy about the excruciating nerve pain and chronic muscle fatigue and weakness issues that developed, all due to the toxicity of treatments. I also suffered a loss of my fertility from a surgery that helped to cure me, which wasn't easy either. Fighting cancer left my body permanently scarred in dozens of ways.
The real scars however, were those within. It's tough to go from thinking that you have your entire life in front of you, to wondering if you're still going to be a free person, or have a life to live at all if your next round of monthly scans don't come back clear. We want to be free, and we want to know that our bodies are rid of our cancers forever, but you never really know. The uncertainty can eat you alive inside, and mental health issues such as depression are common. The anxiety about cancer tends to worsen in the years after fighting, because we live our lives constantly watching over our shoulders. We worry about every little pain in our bodies, because once you've had cancer, every such pain could mean the possibility that our cancers are back.
I became so spooked that my cancer had returned at one point, that it opened the floodgates to all of the terrible emotions that I had kept locked away when I was fighting cancer. I began suffering from post-traumatic stress, which puts the feeling of panic inside of you as though your house were on fire, except you have nowhere to go, and no avenue of escape. My body had betrayed me in the most terrible of ways, cheating on me with death at such a young age. I was terrified of living in my own skin and body. I wanted to run away from it all, but how do you run away from your own body? You can't escape it, or could you?
I was hurting so badly inside, that I contemplated suicide as a means of escape. My wife needed me. My children needed me. My family and friends needed me. I didn't do it, but I had to find a way to end this pain, and doing that wasn't easy either.
It took the support of the cancer community, some wonderful friends and mentors whom I will love for the rest of my life, the unconditional love of my wife who has never left my side, my family, and my two totally awesome children to help pull me through such a terrible ordeal. Not one single aspect of what I've been through could ever be considered easy. Everything has been hard, and I've had to reinvent myself and my life three times over since my cancer fight ended, all from an "easy" earlier stage "good risk" cancer with a 95% cure rate. A high cure rate is wonderful, but finding my way through these past five years after cancer have been the hardest five years of my life.
There is no easy cancer.
StevePake.com
What Cancer Surveillance and Scanxiety Feels Like
25 Appointments and Counting... On the eve of my 4 year check-up for cancer, I rather foolishly clicked on a news video link of Virgin Atlantic Flight VS43's emergency landing in Gatwick last December. I've watched emergency landing videos before, but this is just asking for trouble around surveillance appointments, and I should have known better. As the Boeing 747-400 came down without its starboard main landing gear deployed, and with emergency vehicles lining the runway that were prepared for the worst, it was as though all of the collective fear, anxiety, and tension of the passengers on-board that aircraft found a way to channel straight through me. I could relate to this so well, because I know exactly what this feels like, and it's how I had already been feeling at the sub-conscious level. This is what I've been going through for 4 years now, over and over again, as an 'S.O.S.' cancer patient, "stranded on surveillance."
25 Appointments and Counting...
On the eve of my 4 year check-up for cancer, I rather foolishly clicked on a news video link of Virgin Atlantic Flight VS43's emergency landing in Gatwick last December. I've watched emergency landing videos before, but this is just asking for trouble around surveillance appointments, and I should have known better. As the Boeing 747-400 came down without its starboard main landing gear deployed, and with emergency vehicles lining the runway that were prepared for the worst, it was as though all of the collective fear, anxiety, and tension of the passengers on-board that aircraft found a way to channel straight through me. I could relate to this so well, because I know exactly what this feels like, and it's how I had already been feeling at the sub-conscious level. This is what I've been going through for 4 years now, over and over again, as an 'S.O.S.' cancer patient, "stranded on surveillance."
Virgin Atlantic Flight VS43, a Boeing 747-400, makes an emergency landing at Gatwick in December of 2014, without it's starboard main landing gear (outboard) after circling for hours burning off fuel.
Nobody chooses to get on an aircraft that's going to have an in-air emergency. Who would possibly make such a decision, and how could you possibly know? Nothing like this was ever supposed to happen to you, yet there you are, settling in for your flight as the Captain comes on the PA system, announcing that there's been a landing gear malfunction, and that you might not be able to land safely. As in, we all might die. Your heart skips a beat. The words "you have cancer" are similar. All of a sudden, all that you've been working towards, and all of your hopes and dreams are, literally, up in the air. Your future, including weather you'll even have one or not, is now entirely dependent on weather you're able to get off of this plane alive or not. You're absolutely trapped and helpless, and there's not a damned thing that you can do about it.
The worst part is the waiting, circling the airport for hours while tens or even hundreds of thousands of pounds of fuel are either burned off or dumped, and the pilots exhaust every option they have trying to free the stuck landing gear. Flying around for hours reduces the weight of the aircraft as much as possible as fuel is burned off, which minimizes potential structural stress on landing, not to mention flammability. The wait is excruciating, but increases the odds of survival. Yes, survival. You could spin out of control on landing, or go up in flames. It really puts things in perspective for you when your life is on the line like this. That time spent in limbo gives you a lot of time to think about life, and what's truly important to you. It's the same for cancer survivors getting scans and blood tests done, and then having to wait forever to know the results. Back on the aircraft, the tears really start to fall when you start flipping through photos on your phone of your kids, your spouse, and your family and friends, wondering if you're going to live or die, and if you've already seen them for the last time or not. It's slow and agonizing mental torture.
Hours later, the moment of truth finally comes. You're on final approach, and emergency vehicles are ready. Either the pilots will be able to safely land the plane, or they won't. Either your scans and tests are going to come back clear, or they won't, and all you can do is pray. Feeling so helpless and out of control like this is what finally brought God into my life again, and man have I prayed. I haven't just prayed to God in these past few years as a cancer survivor, I've begged and wept so many times. "Please God, let me live for my children," I used to pray over and over again through tears. But most suddenly and unexpectedly, you hear the engines surge and you start gaining altitude? What's going on?? That familiar "dong" chimes, and the Captain comes on the PA system, terribly apologetic. "Sorry folks, but there's going to be another delay. There's a scheduling conflict - your oncologist isn't going to be in the office that day, and we need to move your appointment to next week." Ugh! But I had been spooked and finally managed to mentally prepare myself for this moment. You mean, now I'm stuck twiddling my thumbs in limbo for another week, and am going to have to go through this wretched mental process of preparing for what could potentially be my last moment all over again? F*ck me!
This is my twenty-fifth time going through this now.* That's twenty-five emergency landings. Each time it's a a little different, but still very much the same. It gets easier with time, but is it ever really easy? We get nervous and irritable, our moods sour, our anxiety levels go through the roof, and our imaginations run wild sweating every little ache or pain. We might become withdrawn and not really want to talk to anybody, as I have now as I write this. My wife and I both recognize this all too familiar pattern by now. My emotions are being held hostage again, and I'm going to be circling the airport for quite a long time before yet another emergency landing.
"There's a zillion reasons to be having strange pains in your body, but when you've had cancer, all you can think about is that your cancer is back."
I somehow kept making it through these moments for awhile, but after my fifteenth emergency landing at the end of 2012, I completely lost it. I was so spooked and afraid, and thought for sure that this was going to be the time that I would finally go up in flames, or maybe crash into the water and drown? There were so many strange things going on with my body, along with some other bad omens in the world that had spooked me. I was fine. Extra tests that were done came back negative. There's a zillion reasons to be having strange pains in your body, but when you've had cancer, all you can think about is that your cancer is back.
US Airways Flight 1549, successfully ditched in the Hudson River in January of 2009. Imagine having to go through something like this every other month.
Maybe this one was a bit like US Airways Flight 1549, when Captain "Sully" Sullenburger famously had to ditch his Airbus A320 in the freezing Hudson river in January 2009, after losing both engines to a dual bird strike. Miraculously, everyone survived, but man did I sink. That one broke me. I just couldn't go on. I was so done. I couldn't do this anymore. I just wanted to run away from life and let whatever was going to happen to me happen, but my network of supporters lifted me with their love, and carried me when I could go no further myself. I was alive and breathing, but drowning in cold and traumatic memories of all that I had been through, that I had somehow managed to keep locked away and repressed up until that point. After that time, and that landing, it all started pouring out. On my sixteenth emergency landing, two months later in February of 2013, I was so emotionally blown out from feeling so much, that I couldn't feel anything at all for awhile. I was still numb and broken. After my seventeenth emergency landing in April of 2013, I sat in my car and just cried for a half hour afterwards. I was so happy and relieved to be alive, despite the fact that this was killing me, too. I just needed this all to be over with, but knew I still had such a long ways to go, and that I would have to find better ways of dealing with this pain.
It's not my five-month long fight against cancer that's marked me and changed me as a person, but rather the repeated emotional trauma of one emergency landing after another in the years after on surveillance. Every single time, it's the same feelings of endangerment, yet having nowhere to run and nowhere to hide, and just having to wait it out. It's ironic how these rigid surveillance protocols are designed to catch recurrences of our cancers as early as possible, and give us the best chance of survival after decades of accumulated medical knowledge, yet the extreme stress that the protocols themselves bring on can kill us at the same time. Mental health issues such as post-traumatic stress and depression are common in cancer survivors, and it came as no surprise to me whatsoever that post-traumatic stress is common in airline passengers that had been involved in emergency landings as well. Sadly, even suicides were common for the first generation of young adult cancer survivors, in the absence of all of the knowledge and support that we have today in the connected world. It's always been a blessing to be alive, but it's been a hard life to live.
The thorn in all of our sides is that we never really know if our cancers are gone or not. Passage of time without any new evidence of disease is the only thing that proves that we're cured. It's not the surveillance that kills us, but rather living with so much uncertainty all of the time, and the constant reminder of just how fragile our lives have become. We want to know that we're going to be healthy and that we'll never get sick again, but there's never been a guarantee for anybody. It's a false sense of security about life that we lose after cancer, and we never get that back again. It's been so hard learning to live without that.
"No cancer survivor should ever be left alone and without support."
A successful cancer survivorship is marked by our abilities to adapt to our new lives, to find outlets that help us cope and relieve this extreme stress, and by finding the support that we need. This can't be done alone, and no cancer survivor should ever be left alone and without support. Consciously, I know that there's little reason for me to be so afraid at 4 years out, as my surveillance appointments are mostly a formality by now. It's post-traumatic stress and my defensive instincts kicking in that's causing me to be this way, so withdrawn, irritable, and tense. It's that same feeling of dread coming back to the surface, as you approach yet another emergency landing. We can't just turn off our instincts. Oh, how much easier life could have been these past few years if there was just an 'off' switch for this, but these are hard-wired into us and they're always on, always alert, and some of us have stronger defensive instincts than others. We have to find ways to work with these defensive instincts of ours, and so I run. I run as hard as I can go at times, consequences be damned. I write, I spend plenty of time with family and friends, and never stop LIVING in between these emergency landings. Doctors and well-meaning friends will say that you'll adjust to a "new normal" after cancer. They haven't the slightest clue what they're even talking about, but this is it. Welcome home.
As VS43 touched down, almost teetering on the edge of balance as the pilots delicately applied flight and then ground controls without its starboard main landing gear deployed, a passenger can be heard weeping on an in-flight video that someone took as the aircraft finally rolled to a stop. It's such a different situation, yet emotionally, exactly the same as what we go through as cancer survivors on surveillance. Who would volunteer to do this over and over again, if somehow they knew a flight was bound for trouble? They'd rightly be called a fool, a daredevil, or an adrenaline junkie not long for this world. I'm not one of these people and never have been, yet this is my life on surveillance after cancer. We endanger ourselves for real if we don't subject ourselves to this, but it can easily overwhelm and push our mental sanity far beyond our limits when we do. Going through this broke me as a person, forcing me to rebuild my life from the ground up in order to accommodate such extreme stress and pressure. Sometimes it takes everything I have to just survive, and I have to utilize every source of support and coping mechanism that I've developed just to get through some days. A well-stocked liquor cabinet, or in the galley on the plane, is your friend, too.
Here we are at last, on final approach for real this time, emergency landing cancer surveillance check #25. Some deep breathes and a final prayer said, and one last "F*ck You, Cancer!" just for good measure. What will happen this time? You just never know, and have to learn to live with the uncertainty and your life being constantly thrown up in the air like this as best you can. 100 feet, 50 feet...here we go again.
Brace! Brace! Brace!
StevePake.com
* My cancer surveillance protocol by Memorial Sloan-Kettering Cancer Center for Stage IIB non-seminoma testicular cancer, treated successfully with combination EPx4 chemotherapy and the RPLND surgery, is the most aggressive (conservative) I've ever heard of. I've had H&P, blood tumor marker checks, and a chest x-ray every month for the first year, every two months for year 2, every three months for year 3, and every four months for year 4. These short intervals are what help to detect a potential recurrence as quickly as possible, which gives the patient the maximum odds of survival. It's part of why testis cancer centers of excellence like MSKCC have the highest survival rate for testicular cancer in the world. I would never even think of becoming non-compliant, but the rigors of being on such an aggressive surveillance protocol have certainly left a mark, and taken a huge emotional toll on me.
The Truth About Testicular Cancer Markers, and Detection with Pregnancy Tests
It seems like every few months, a story pops up somewhere where somebody managed to detect their testicular cancer with a pregnancy test. Yes, it's true! Thiscan be done. In a strange coincidence of nature, the hormone called beta human chorionic gonadotropin, or HCG for short, which is emitted from the cells that form the placenta when a woman is pregnant and is what the pregnancy test looks for, can also be emitted by some types of testicular cancer. Since HCG should never be elevated in men except for in a few rare and very specific situations, a positive pregnancy test result in a man is almost a sure sign of testicular cancer!
It seems like every few months, a story pops up somewhere where somebody managed to detect their testicular cancer with a pregnancy test. Yes, it's true! This can be done. In a strange coincidence of nature, the hormone called beta human chorionic gonadotropin, or HCG for short, which is emitted from the cells that form the placenta when a woman is pregnant and is what the pregnancy test looks for, can also be emitted by some types of testicular cancer. Since HCG should never be elevated in men except for in a few rare and very specific situations, a positive pregnancy test result in a man is almost a sure sign of testicular cancer!
The latest story on this is that of Byron Geldard, from Huntingdon, Cambridgeshire in the UK, first reported in the Daily Mail, and then The Telegraph, Liftbump, and other UK based media outlets. The problem with many of these stories is that an incomplete truth, or even dangerous misinformation can often emerge. In Geldard's story, the Daily Mail had it correct and quoted Dr Danish Mazhar, Consultant Medical Oncologist at Cambridge University Hospitals, who said: "The pregnancy hormone (HCG) is often (but not always) produced by testicular tumours," meaning that a simple pregnancy test is not a foolproof test for testicular cancer. Other types of testicular cancer tumors produce another type of marker called alpha-fetaprotein, or AFP, which the pregnancy test won't detect. A third type is an enzyme called lactate dehydrogenase, or LDH, which is not reliable enough to be used as a primary indicator for testicular cancer, but is commonly used as a secondary one to gauge the extent of disease. Guess what? The pregnancy test doesn't look at this either, and it's also possible to have testicular cancer that doesn't give off any markers at all.
Which types of markers the various types of testicular cancer may or may not give off are known and very well understood. There are two main types of testicular cancers, which are called seminomas and non-seminomas. Seminomas are very simple, and 95% of the time are the classical seminomas. Non-seminomas are a bit more complicated, and are divided into embryonal carcinoma, choriocarcinoma, yolk sac, and teratomas.
Seminoma can occasionally give off HCG, but never AFP.
For non-seminomas:
Embryonal Carcinoma can give off HCG and/or AFP, but might not give off either.
Choriocarcinoma always gives off HCG.
Yolk Sac almost always elevates AFP, but in rare cases might not.
Teratomas do not give off either type of marker.
With the exception of seminomas, testicular cancer tumors are rarely a pure type. Non-seminomas are commonly mixed with another non-seminoma type of the cancer, or a seminoma, to form a mixed germ cell tumor. Information like this is good to keep handy because of the fact that testicular cancer is still considered a relatively rare cancer, which means there are a lot of oncologists out there that just aren't that familiar with the disease. If your pathology report says 100% pure seminoma, but your lab results are showing elevated AFP, it's a sign that something might have been missed in your pathology and that you need to get a second opinion!
As you can see, properly detecting and diagnosing testicular cancer is a bit more complicated than just taking a pregnancy test. There's only one sub-type of testicular cancer that a pregnancy test will detect every single time, and that's choricarcinoma, but which tends to be more rare. It's a crap shoot with all of the other sub-types, as only some "can" emit the HCG marker, and others won't do so at all. Reader beware! Any article or story you see discussing how testicular cancer was detected with a pregnancy test that only talks about HCG, but makes no mention of AFP, or the possibility of no markers at all, are not giving you a complete set of information. And any story that suggests or implies the reliability of a pregnancy test for diagnosing testicular cancer without mentioning other required tests, is dead flat wrong, and very dangerous misinformation. If you suspect testicular cancer, don't 'Net MD' yourself into thinking you're okay if you take a pregnancy test and it turns out negative, because a pregnancy test hardly represents a proper work up for a patient that could have testicular cancer.
If you suspect testicular cancer and take a pregnancy test,
a negative result can NOT, by itself, rule out testicular cancer.
My personal pathology was 90% embryonal carcinoma and 10% yolk sac mixed germ cell tumor, but my cancer emit neither HCG nor AFP! My LDH was slightly elevated, but considering I was injured at the time (from doing something incredibly stupid, I might add), it could have just as easily been elevated from that as it could have from cancer. We'll never know. With my primary HCG and AFP markers always having been negative, the only way to track my cancer during treatments and on surveillance has been radiologically. I still get blood draws and tumor marker checks at every surveillance appointment for HCG, AFP, and LDH, but they're more useful for potentially catching a second testicular cancer (knocks on wood) that might just happen to elevate one of the markers, than it is for tracking my previous cancer that never emit any. Had I depended on a pregnancy test to tell me if the ache in my right testicle was cancer or not, and then brushed off a negative result for a few months until more severe symptoms appeared, I might not be here today! Luckily, I was smarter than that, and you should be too.
I spoke to Michael Muriett, Testicular Cancer Awareness Foundation Vice President and Director of Education, who had the following to say. "We walk a very dangerous line when information like this is published in mainstream, and even more so in Social Media. The impression is given to these men that there is a quick and easy solution. Publishing stories like this without the additional, medical based, factual information in regards to tumor types, cancer marker levels, and how they can be effected can give a false sense of security to people. The best, and wisest route to take will always be consultation with a doctor, cancer screening from that doctor or a hospital, and promoting things like the monthly TSE for early detection."
Although neither the Daily Mail or The Telegraph mentioned the AFP marker, they both did a reasonably good job, assuming one read the entire article, of making it pretty clear that a pregnancy test isn't a foolproof test for testicular cancer, but can be used as a diagnostic tool. Things went terribly wrong at LiftBump however, where the author, 'Katie', with no contact information posted, completely misquoted the Trust spokeswoman mentioned in The Telegraph piece. The LiftBump piece said, "A spokeswoman for the Trust told the Telegraph that a pregnancy test can be used to diagnose, or rule out, testicular cancer, because the disease produces the same hCG hormone that is produced by a developing placenta." Wrong. They never said that. It can produce the HCG hormone, but might not, and the spokeswoman clearly stated in The Telegraph, and even quoted in LiftBump that, "if [a pregnancy test] is negative, it just means that further tests are needed." Yet somehow, LiftBump managed to add into the spokeswoman's statement that a pregnancy test could be used to "rule out" testicular cancer. That is absolutely dead flat wrong. It can not, and this is incredibly confusing, misleading, and dangerous misinformation that has now been shared 24,000 times over on Facebook, with 415,000 views as of 10PM Eastern on March 12th, 2015. Unbelievable. And yes, the LiftBump piece being shared on social media is how I personally first saw this story.
As always, know the signs and symptoms of testicular cancer, and keep doing monthly self-exams. If you detect a mass or have other signs and symptoms, feel free to take a pregnancy test, but please do the proper thing and get to a doctor immediately regardless of what any pregnancy test might say. They simply are not a reliable diagnostic tool for detecting testicular cancer by themselves. Properly working up a patient suspicious for testicular cancer requires the care of a doctor, and for other tests to be run. Even Snopes says so.
StevePake.com
Doctors Say, Keep Checking Your Nuts
In February 2015, Steven Petrow published an article in the Washington Post titled "Guys, here’s why it’s not worth testing yourself for a ‘lump’ down there", coming out against testicular self-exams (TSE) after having previously been supportive of them. What's surprising about the article is not just that such a view against testicular self-exams exists, but because Mr. Petrow himself is a twenty years and change survivor of advanced stage testicular cancer. I applaud and congratulate Mr. Petrow on reaching such a milestone. It's something that we cancer survivors take great pride in and stories like his are inspiring to so many of us, but I could not disagree more with his recommendation against TSE. Petrow thinks that it's "smarter" now to keep his hands to himself, but is it really?
In February 2015, Steven Petrow published an article in the Washington Post titled "Guys, here’s why it’s not worth testing yourself for a ‘lump’ down there", coming out against testicular self-exams (TSE) after having previously been supportive of them. His article responded to a "Today" show segment which aired late in 2014 featuring David Samadi, who is Chairman of Urology and Chief of Robotic Surgery at Lenox Hill Hospital, and is also a Fox News Medical Correspondent. On the "Today" show episode, Samadi gave testicular exams to anchors Willie Geist and Carson Daly on live television. What's surprising about the article is not just that such a view against testicular self-exams exists, but because Mr. Petrow himself is a twenty years and change survivor of advanced stage testicular cancer. I applaud and congratulate Mr. Petrow on reaching such a milestone. It's something that we cancer survivors take great pride in and stories like his are inspiring to so many of us, but I could not disagree more with his recommendation against TSE. Petrow thinks that it's "smarter" now to keep his hands to himself, but is it really?
Why Is there Even a Debate?
The original source of the recommendations against doing testicular self-exams comes not from Petrow, but rather from the US Preventive Services Task Force (USPSTF). The USPSTF recommended against testicular self-exams back in 2012, citing "moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits". In his article, Petrow spoke with Kenny Lin, assistant professor of family medicine at Georgetown University Medical Center, who agreed. Lin said that even if self-exams were effective, that they'd have "little if any bearing on outcomes for those who are diagnosed." Lin went on to say that he thought the "Today" show episode was "a stunt cloaked as a health message." Petrow went through a brief discussion of benefits vs harm, but couldn't seem to find any benefits at all for the TSE. Much of the rest of the piece then focused on psychological biases as to why doctors (and patients) would still want such screenings despite there being "no benefits". Well, maybe they're looking at things the wrong way.
Problems with the Recommendation Against TSEs
One of the biggest problems with Petrow's article is the fact that no matter which type of cancer he was discussing, there was no mention whatsoever of cancer survivorship quality of life, or the overall wellness of a patient after cancer. He only looked at "surviving" cancer from the singular perspective of the net final outcome - whether the patient lived or died in the end. Because the "final outcome" isn't likely to change, don't bother with screenings or self-exams, goes this line of logic. If you get cancer, just go get chemotherapy or radiation, or whatever it is that you need, and get cured. As I wrote in my own lengthy blog post on this exact topic in June of 2014 titled, "The Value of Testicular Self-Exams and Early Detection from the Survivorship Perspective" this is a woefully incomplete, and dare I say even irresponsible perspective. We're so much more than just a binary "1" or "0" on someone's spreadsheet on whether we're alive or dead. We're very much analog creatures, and cancer survivorship itself is a million shades of gray.
Petrow stated in the article that he went through 4 rounds of chemotherapy and two surgeries to get cured, but didn't mention what, if any, long-term or possibly permanent side-effects he might have suffered as a result of this. As I wrote in my own blog last year, the potential for long-term health risks and permanent side effects when going through treatments for cancer are not to be underestimated. I've suffered a complete loss of fertility, for starters. Not having much if any feeling in my left foot is more minor and something that I've gotten used to over time, but more severe is the fact that I also suffer from chemo-induced peripheral neuropathy. I deal with chronic muscle fatigue issues to varying degrees every single day, and continue to have nerve pain issues that have never really gone away completely. Even after my cancer fight was over, I still had to keep fighting because one of my kidneys nearly failed due to a complication from the RPLND surgery that I went through. It took another year after my cancer fight, and tons of painful diagnostic procedures and stents to finally nurse my body and my kidney back to health. Even more troubling are the increased risks of developing a secondary cancer just from having been exposed to chemotherapy agents and/or radiation treatments. Patients who are exposed to either chemotherapy or radiation therapy have a two-fold increased risk of developing a secondary cancer compared to the general population, and a three-fold increased risk if a patient has been exposed to both types of treatments, according to studies. Mental health is also at stake. After fighting so hard, my mind eventually caught up with all that I and my body had been through, and I fell into a depression and suffered from post-traumatic stress for a year.
Testicular cancer tends to hit younger men, like myself, who have so much of their lives in front of them. They're going to have to live with these potential long-term side-effects of treatments for quite a long time, which is why it's so important to detect testicular cancer as early as possible. The earliest possible detection of cancer helps to minimize the amount of treatment needed, the potential trauma to both mind and body, and helps to maximize quality of life after cancer. It's important to be a "1" on that spreadsheet and to survive, but we can't take our eye completely off of the ball when it comes to the impact on quality of life that cancer treatments can have. Why would you not want to detect a cancer as early as you can via something as simple as awareness of the disease itself, and a virtually zero cost TSE? Is it really in the best interests of the general population to have people darn near on their death beds before being properly diagnosed? It doesn't make sense. Especially with testicular cancer, a rapidly advancing cancer, a pain or mass detected in the testicle via a TSE might be the only sign of testicular cancer one has before its had the opportunity to completely overrun one's body. This is why testicular cancer is sometimes referred to as the silent killer!
What Some Experts Really Think
One really needs to understand what's behind these USPSTF recommendations against many types of screenings. A trip across the Beltway and up the Baltimore-Washington Parkway from Georgetown, is The Johns Hopkins University in Baltimore. Philip M. Pierorazio is an Assistant Professor of Urology and Oncology at the Brady Urological Institute there, and Director of the Division of Testis Cancer (Pierorazio is also a member of the TCAF board of directors). Pierorazio weighed in on the USPSTF recommendations on his own blog in a piece titled "Testicular Self-Exam: Why There Is Nothing Wrong with a Regular Feel". He writes,
"It has to be conceded that there is no evidence that TSE is effective for the diagnosis of testicular cancer or helps find men at an earlier stage of disease. However, lack of evidence does not mean that TSE is not effective – it means that no study has effectively investigated the role of TSE in an at-risk population." Dr. Phil Pierorazio
In his summary, Pierorazio respectfully disagreed with the USPSTF recommendations, stating that the recommendations are themselves based on very little existing evidence. "While the cure rate of testicular cancer is wonderful, the burden of the disease is greatly under-appreciated. Even if a free, painless self-examination leads to an unnecessary doctor's visit, saving one man from advanced disease is well worth the "risks and costs" of TSE.", concluded Pierorazio. In case you didn't follow, the issue is simply that there just hasn't been a formal study done to prove the effectiveness of TSE. It doesn't mean that they don't work or aren't effective. It just hasn't been proven that they're effective via a study. Thus, in the absence of a formal study either proving or disproving effectiveness, the USPSTF recommendation to "discourage the use" of the TSE is based on very little evidence as well!
I had a chance to speak with David Samadi personally on Petrow's article, and that "Today" show segment. Samadi shared the sentiments of Pierorazio and myself but in a slightly more vocal manner, stating that he felt the USPSTF recommendations against the TSE and screenings for other types of cancers were "a terrible mistake". While some of these screenings might not be perfect, he and others believe they're still effective tools that can change the final outcomes for patients, and that it's always better to catch a cancer at an earlier stage to minimize the treatments needed to cure a patient. I shared my personal story with Samadi, and that I had missed being able to pickup on my symptoms of testicular cancer for a few months. If only I had been more aware of the disease and how to do a proper TSE, I potentially could have caught my cancer at an earlier stage, and spared my body and my mind from the harsh treatments that were needed for me to get that cure. Samadi's response? "Exactly." Samadi went on to say in a statement.
"Given how common testicular cancer is in young men, we should be urging them to perform monthly self-exams. Young women are encouraged to perform monthly self-breast exams. Why shouldn’t men? Early detection begins with the patient. If he is aware of the risk factors, he will care about prevention. Self-exams are a no cost prevention method and if something is discovered, a simple ultrasound can tell us what’s happening." - Dr. David Samadi
I agree with that this is a double-standard, and had mentioned it myself. Women are encouraged to get to know the shape and feel of their breasts, but men are supposed to keep their hands off of their balls?
There's no finer authority on testicular cancer anywhere in the world than Lawrence Einhorn, a Distinguished Professor of Medicine and Lance Armstrong Professor of Medicine at the Indiana University. "Einhorn" is a household name in the oncology world, and a man who needs no introduction. Einhorn's work at Indiana University 40 years ago experimenting with the Cisplatin drug is what turned testicular cancer from a death sentence into the greatest success story in modern oncology, having been compared with walking on the moon! Einhorn's work has literally saved the lives of hundreds of thousands of men with testicular cancer, my own included. I reached out to Dr. Einhorn and asked if he could weigh in on the USPSTF recommendations against the TSE, asking if "men should really be discouraged from doing testicular self-exams?" Einhorn's response? "Not really." He went on to express skepticism on the effectiveness of a national policy for TSEs, citing the low overall incidence rate of testicular cancer, but he couldn't have been more clear on the importance of knowledge and awareness of the disease.
"Men should be aware there is cancer that can start in the testis and the presence of pain or a feeling of firmness in the testis should not be ignored", stated Dr. Einhorn.
I don't think there's a finer endorsement to be had on the topic of testicular cancer awareness and the TSE than from Dr. Einhorn. Men need to be educated and aware of the possibility of testicular cancer, and how to properly feel for any abnormalities via a TSE!
Move Forward With Education & Awareness, Not Backwards with FUD
The solution to the potential downsides of TSEs, such as the cost of false positives and fear and anxiety, is not to forego TSEs altogether, but rather to help minimize them with education and awareness. This is precisely what organizations like The Testicular Cancer Awareness Foundation are all about. We teach people about the signs and symptoms of testicular cancer, which will help men of all ages to understand what to look out for. Knowledge of how to do a proper testicular self-exam will help to familiarize them with their own anatomy, and establish the difference between normal and abnormal. Knowing all of this can help to minimize unnecessary office visits and expense, and cut down on stress and anxiety.
As for the true costs when an office visit is needed, Pierorazio weighed in on this in his blog also, citing a University of Kansas Medical Center study. The cost to treat an advanced stage testicular cancer with both chemotherapy and the RPLND surgery is equivalent to hundreds of office visits to look at a worrisome TSE. When cancer is detected (and actual masses that are detected in the testicle are almost always cancerous), the costs to treat earlier stage cancer enabled by awareness of the disease and TSEs, is a mere fraction of the costs to treat advanced stage testicular cancer. A mass can't always be detected in the testicle by self-exam in testicular cancer patients (a proper study on the TSE would help to better understand this), but in my case I did, and I wished I had given it a proper feel a few months earlier when it would have been at an earlier stage. Instead, my cancer advanced for several months to the point that I had to be treated with both chemotherapy and the RPLND surgery, and at great cost both in terms of the dollars required, and the impact to my body. A few ultrasounds that turn out negative are a drop in the bucket.
The "Cost" of Getting to a Doctor Too Late When It's Cancer
If there's one thing that I think most all of us could agree with Petrow on wholeheartedly, it's the fact that many men, and especially young men and boys, can be just plain shy or too embarrassed to talk about potential issues with their bodies when they notice them. In Petrow's article, he shared the story of one of his own doctors, who developed a case of hemorrhoids. Even his doctor was embarrassed, and delayed getting it checked out. Samadi would agree with the reluctance of men to go see doctors as well, and says it's not men but rather women who end up being the ones who finally get men into his office. "If you want a job done right, you give it to a woman,” said Samadi in a Forbes article. "Women are the most proactive healthcare champions in the family and are the driving force in men’s health. Time and again, it’s women who make the final push for their husbands, fathers, and brothers to come see me.” But we're talking about cancer screenings here, not hemorrhoids. The consequences of not getting to the doctor on time for what could potentially be cancer can be deadly.
In a call for comments on this topic on a testicular cancer support group, there were no shortage of comments from those who had lost loved ones, or those whose quality of life had been impacted. If only they could have picked up on the cancer sooner with either more awareness about the disease or with self-exams, maybe their loved ones might still be here, or their quality of life might not have suffered as much. In one post, Melia Elliot shared the tragic story of her son, Ben. As Ben grew into puberty he had noticed that one testicle grew larger than the other. Ben 'Googled' that this could be normal, and then never said a word to anybody. When other symptoms started to appear, a sign of very advanced stage testicular cancer, he was unfortunately misdiagnosed for nearly two months by doctors in their hometown of Joplin, MO, even after an ER visit and two follow-ups. It wasn't until Ben became paralyzed from the chest down that doctors finally realized that he had testicular cancer! Not trusting the doctors in Joplin to care for her son, she got Ben up to Kansas City where Peter Van Veldhuizen, who is a Professor of Internal Medicine and Director of the Hematology/Oncology Division at The University of Kansas Medical Center, started Ben on BEPx4 chemotherapy for advanced stage disease.
It turns out that I had conversed with Melia personally during this time via one of the Testicular Cancer support forums on the web. It sounded like the BEPx4 might not have been working, and I recommended that she get her son under Einhorn's care at Indiana University STAT. Ben's case sounded so dire that I insisted that she call Einhorn's office that day, and that it couldn't even wait until tomorrow. Too many mistakes had already been made prior to Ben's diagnosis, and too much time had already been lost. She made the call to Einhorn's office immediately, and Ben was rushed to get started on high-dose chemotherapy with stem-cell transplant under Van Veldhuizen's care and with Einhorn's guidance. Melia stated to me in a comment that the quality of care between Van Veldhuizen and Einhorn was exemplary, but it was just too late. Ben fought a hard and courageous battle, but died tragically 10 months from his diagnosis.
Testicular cancer is curable, but it's also a killer! Someone dies of the disease every day, and on that day it was Ben. Early detection remains the key, and knowledge and awareness about testicular cancer is so important, especially with teenage boys!
Guys, Keep Checking Your Nuts
Pierorazio's statement bears repeating. "lack of evidence does not mean that TSE is not effective – it means that no study has effectively investigated the role of TSE in an at-risk population." The recommendations by the USPSTF are themselves based on very little existing evidence. When prominent doctors with expertise specifically in testicular cancer continue to believe in the TSE despite what the USPSTF has said, I think the message is pretty clear.
All of us in the Testicular Cancer advocacy world know what the true "cost" is when you're too late. For Melia Elliot and her son Ben, the price was far too great. Samadi sums things up well in his bottom line. "Encouraging men to be more aware and preventive when it comes to common cancers could be the only chance we have to save their lives.” Women especially know just how stubborn men can be. Along with Dr. Samadi, we encourage women to be proactive and get involved in men's health issues. Take the #SamadiChallenge for Testicular Cancer and make sure that the men in your lives including your children are aware of men's health issues that could affect them, encourage them to perform self-exams, and seek the care of a doctor immediately if they notice something abnormal. And most of all...
Keep checking your nuts!
The doctors who really know Testicular Cancer say to.
StevePake.com
Special thanks to Melia Elliot for her willingness to share the story of her son, Ben. Ben passed away on August 22, 2014.
Cancer Survivorship - The Fight after the Fight and All of its Firsts
After our fights with cancer are over, we all want so badly to believe that everything is behind us and that life is going to get back to normal. Those first weeks and months after our cancer fights are such a precious time. It’s our first taste of freedom after having been wrongfully held hostage by cancer for so long. I had my life back, but as time and the months went on I realized that it wasn’t my old life that I had back, but rather an entirely new one. Cancer survivorship brings with it an entirely new set of life circumstances and a whole lot of firsts, many of which I was completely unprepared to handle or to deal with at all.
I thought I was all done with cancer here. I was really just getting started.
After our fights with cancer are over, we all want so badly to believe that everything is behind us and that life is going to get back to normal. Those first weeks and months after our cancer fights are such a precious time. It’s our first taste of freedom after having been wrongfully held hostage by cancer for so long. I had my life back, but as time and the months went on I realized that it wasn’t my old life that I had back, but rather an entirely new one. Cancer survivorship brings with it an entirely new set of life circumstances and a whole lot of firsts, many of which I was completely unprepared to handle or to deal with at all.
For the first time in my life after my cancer fight, I was genuinely afraid. Gone was that false sense of security that we all tend to have about our lives and our health, especially as young and invincible adults, replaced with incredible feelings of insecurity. My cancer fight had stripped me bare of all of this false security, and I felt naked, afraid, and vulnerable. It’s not something you dwell on during the actual cancer fight because you’re so focused just trying to survive and get through each day. It tends to hit you later after your cancer fight, it never really goes away, and it's terrifying that you never really feel safe like you always had before.
For the first time in my life, I also had to deal with some pretty serious secondary health issues. As a result of chemotherapy and a complication from a surgery, one of my kidneys nearly failed. On one hand I was happy just to be alive and took it in stride as the price of the cure, but on the other hand I was frustrated and disheartened, and in a lot of pain for quite a long time. The one and only body I’ll ever have had just taken the beating of its life at only 33, and I began to worry about what life might be like as I aged, and what my quality of life would be like if I faced another health crisis. I worried that my body wouldn’t be able to handle it, and this just added to the existing feelings of vulnerability and insecurity.
For the first time in my life, I learned what an emotional roller coaster was in the form of cancer surveillance checkups. Suddenly we go from living a normal life and dreaming and working towards wherever we want to be in 5, 10, or 20 years, to just trying to get through our next set of scans a month or two down the road. The thorn in the side of every cancer survivor is that we never really know if we're "cured" or not. The passage of time without any new evidence of disease is the only way we know, and it's a terrible thing to have hanging over your head for so long, and it’s a huge shift in our mentalities especially as young adults.
For the first time in my life, I developed hormonal issues in the form of low testosterone. This resulted in spells of fatigue, depression, mood swings, and low or even zero libido among other things, which could last for as little as a few days or as much as a few weeks. We’re already dealing with insecurities and anxieties about this whole new world that we’ve been thrust into, only to have hormonal issues playing head games with us too! It just piles on, and it’s so cruel and unfair. It was totally not me and a truly awful feeling to be a moody, depressive, lethargic, and asexual lump. It was disconcerting to my wife as well, who had been used to always getting a certain amount of attention from her husband. When that attention suddenly trailed off, she felt self-conscious and wondered if I still loved her, or if I didn’t find her attractive anymore? It was nothing but the hormones talking, or rather not talking!
For the first time in my life, I had a body that would no longer do whatever I asked it to do, whenever I asked. I didn’t get my old body back, but rather a new post-cancer body that needed a whole lot more rest than it ever did, and that no longer had anywhere close to the stamina that it did before. My body had developed permanent symptoms of peripheral neuropathy as a result of my chemotherapy. To this day I cannot really feel my left foot, have limited feeling in my other foot and both hands, and have had to learn to deal with almost constant feelings of muscle fatigue and weakness to varying degrees. Imagine waking up each day and never feeling like you've got anything more than a half tank for the whole day, no matter how well rested you are. It was an entirely new body that I had, with an entirely new set of limitations that I head to learn to respect and stay within, or else suffer the consequences in the form of terrible and nearly disabling fatigue spells.
For the first time in my life, I truly felt loss. I had gained numerous cancer warrior brothers during my fight against testicular cancer, but not all of us were fortunate enough to win our battles. I mourned the loss of each of these friends as if they really were family and brothers. And when one friend passed who left behind his wife and four children, I learned what survivor’s guilt was all about. Why him and not me when I only have two children and he has four? I was so sad, devastated, and felt so guilty that I cried everyday for two weeks.
For the first time in my life, I began to very deeply resent the fact that my wife and I are basically only children, and became extremely jealous of the many people I knew who enjoyed close relationships with their siblings. It was the herding instinct coming to the surface, and the feeling of safety in numbers. I wanted to believe that if for whatever reason I wasn’t going to make it, that our brothers and sisters would be there for my wife and my children, and provide that peer level support and continuance to my family. Instead I felt nothing but a vacuum, which added yet more layers of insecurity on top of numerous other layers of insecurity.
For the first time in my life, I learned that a cancer recurrence scare can be even more terrifying than your initial cancer diagnosis, because all of your naivety and innocence about the brutality of fighting cancer is gone. When you experience a recurrence scare, you're fully aware of the pure hell and world of terror that you could be in for all over again. You know that you've already exhausted the best treatment options and will be on to second and third best options, each with decreasing effectiveness and chances of a cure. When I’ve had recurrence scares, I’ve been so afraid that I’ve cried myself to sleep, only to have terrible nightmares and anxiety that just woke me up again. I was so convinced that my cancer had come back at one point that my death instincts kicked in again. It’s the feeling that this is it, and of needing to tie up loose ends and to say goodbye to people that you love and care about. It was enough to feel these terrible instincts once after my initial diagnosis, but deeply traumatizing to feel them for a second time after a recurrence scare over a year after my cancer fight had ended.
For the first time in my life, I experienced acute extreme anxiety so bad that I’d commonly find myself huddled up in a corner and in tears. I fell into a very deep depression and experienced post-traumatic stress. My terror from the past and worries about the future all combined into one terrifying present, to the point that my mind lost the ability to distinguish real from imagined. Everything and everyone around me felt like a threat that I needed to protect myself from, and my world became very small for a while. I was so spooked and afraid, so tired of my reality of living in constant fear of cancer, and was terrified of living in my own body from which I knew there was no escape. I had had it. I was so done with all of this and just wanted out, but knew that I had to press on. I had beaten the cancer that had taken me hostage, only to have my own mind and its out of control fears and emotions take me hostage during survivorship. I had to learn how to regain control of my mind, and how to master and control all of my fears and emotions, rather than allowing them to control me as they had been. I was ill and hurting so badly inside, but my family needed me. My wife needed her husband, and my children needed their daddy back.
And for the first time in my life, I finally realized just how different life really was after cancer, and how different my needs were as a person. It wasn't just a new life or a new normal after all, but rather a whole new world that I was living in. The terrible anxiety, depression, and post-traumatic stress that I experienced for months over a year into my cancer survivorship was both the very worst thing that happened to me, but also one of the best. It was only then that I realized the need for a complete reset and reboot of my life, and only then that I allowed myself full license to do whatever I needed to do to help myself feel whole, writing people and things out of my life that had been hurting me or just weren't what I needed, and bringing those that were closer.
We do go back to our established adult and young adult worlds after cancer, but we’re also born into this entirely new and terrifying world of cancer survivorship where we’re only just children, and that we’ve only just begun to live in. The way we suddenly lose so much support from all of our doctors and nurses and other medical professionals after we’re declared cancer free, simply because we don’t have anymore appointments to go to, is not unlike abandoning a child in a way! We return to all of the pressures and challenges of our existing lives, but now with all of these new challenges of cancer survivorship, and without the experience and wisdom that age provides to always know how to overcome. We end up having so much growing up to do all over again, but without the benefit of a real childhood in which to learn and explore more freely.
I was declared all clear in July of 2011, but it took me until December of 2013, two and a half years later, to finally feel matured, confident, and secure in both of my worlds. For everything that I’ve faced during my cancer survivorship, there’s always been a way to improve, reduce, minimize, or overcome. There's always been another approach to try, or a new philosophy or way to look at things, and today I enjoy excellent quality of life physically, mentally, and perhaps most importantly spiritually. I know my new body both inside and out, have full control of my mind and all of its emotions and fears, and have finally felt at peace with everything for the past year. This is never something that I or anyone could do alone. It requires a strong village of support for both cancer survivors and caregivers. There are plenty of times throughout all of this, long after my cancer fight had been over, where I've needed a lot of hand-holding, nurturing, and especially the guidance of other cancer survivors or caregivers who had already been there and done that, and could help me find my way. Be those people for us. Be the ones that reach out both to both survivors and caregivers. Be that blessing to us and and check in on us and keep asking how we’re doing. We're only just children again in these first few years as cancer survivors, trying to find our way in a whole new world, and still need every bit of your love and support.
StevePake.com
The Value of Testicular Self-Exams and Early Detection from the Survivorship Perspective
There’s been some debate in recent years about the true value and effectiveness of certain types of cancer screenings.
There’s been some debate in recent years about the true value and effectiveness of certain types of cancer screenings. This is, of course, a perfectly reasonable thing to be doing both in the name of advancing medical science, and especially in an environment where there's so much downward pressure on the costs of healthcare. One of the types of cancer screenings that has been discussed are for testicular exams, and it's been surprising to so many of us in the testicular cancer community to hear that screenings for testicular cancer have actually come back as not recommended or not worth it by some prominent organizations. Consumer Reports magazine even gave the testicular cancer screening one of their infamous little solid black dots, as if it were bad for you and something to avoid! The rationale is that because testicular cancer has such a high cure rate even in advanced stages, that overall survival rates don’t budge significantly whether the cancer is detected early or late. Furthermore, not everybody who is diagnosed with testicular cancer will be able to detect any irregularities in their testicles, which can make it a bit of a hit or miss type of test. So don't worry about testicular exams, some say. If you’re diagnosed with testicular cancer, just go get chemotherapy or radiation treatment or surgery or whatever it is that you need, and get cured.
All of this is perfectly fine and rational from a business and financial analyst perspective, but is completely cold and missing the human cancer survivor perspective on this. We're so much more than just a binary "1" or "0" on someone's spreadsheet on whether we're alive or dead. We're very much analog creatures, and cancer survivorship itself is a million shades of gray. And I have to say, I personally was just a little bit taken aback and offended by the nonchalant manner in which I saw Dr. John Santa, Director of Consumer Reports Health Ratings Center, describing how curable testicular cancer was at any stage, to not worry about self-exams or screening, and to just go get chemo if you're diagnosed with testicular cancer on the Dr. Oz show last year. It made for good TV, and I could sense some pride in Dr. Santa's voice and body language when talking about how curable testicular cancer is these days, as TC is indeed one of the great victories in modern medicine. But it's still a real disease and a real cancer that kills real people. Somebody is diagnosed with testicular cancer every hour in the U.S., and someone dies of it everyday. A cancer warrior brother of mine who had been diagnosed with testicular cancer around the same time as me just happened to be in hospice care and living his last days as this particular Dr. Oz show had aired. To his credit, Dr. Oz defended the practice of testicular self-exams and said he still thought they were a good idea to do, but it was as if I had been punched in the stomach to hear how curable testicular cancer was "at any stage" as my friend was dying of it. And don't believe for a minute that chemotherapy is some sort of miracle pill, and that life will go on just as it had before when it's all done, as that's hardly the case for so many.
My chemo cocktail, Etoposide and Cisplatin for my first round of EPx4, March 2011. Yum yum!!
Testicular cancer is a pretty fast and aggressive type of cancer that can quickly overrun your entire body, but can also be cured completely if it's hit hard and fast. Chemotherapy protocols for testicular cancer are no joke. I'm now casually recalling the movie 'Star Trek IV - The Voyage Home' when Doctor McCoy gives the ailing patient in that San Francisco hospital a pill that miraculously fixed their failing kidneys. I wish it was, but it ain't like that!! The drugs of Cisplatin,Etoposide, and especially Bleomycin that many of us are familiar with are all very serious drugs. There are numerous warning labels right on the bags, and oncology nursing staff handle them with masks on under vented hoods for good reason! They certainly do an awesome job of killing cancer, but they're really not kidding when you read the datasheets for these drugs and look at the potential side-effects that can become long-term or permanent issues. Anybody facing chemotherapy after a testicular cancer diagnosis would be well advised to look at the potential side-effects and risk factors of these drugs, and evaluate them against your personal and family medical history with your oncologist. I did EPx4, and I can personally check the boxes for kidney damage, nerve damage and peripheral neuropathy, and muscle fatigue among other things, along with fertility loss from my RPLND surgery. There's increased risk of developing leukemia with the EPx4 protocol, as well. Potential risks with Bleomycin for the more mainstream BEPx3 protocol are blood vessel damage and Raynaud's, increased risk of heart disease, and potentially nasty effects to your lungs. It's rare, but there are cases of people having beaten testicular cancer, only to end up dying from complications due to Bleomycin. It's not uncommon to hear about cases for people with advanced stage disease who started with BEPx4, but ended up doing BEPx3 + EPx1 either due to complications from Bleomycin (drop in lung function, other severe side effects), or due to getting a good response and just to spare them from the additional Bleo exposure. These drugs are no joke!
In my case, I might have been able to avoid much of what I went through if only I were more aware of Testicular Cancer. I started having strange pains in my right testicle two months prior to my diagnosis, but passed it off until the pain finally got so bad that I couldn't even sleep at night. I had not even considered the possibility that this could have been cancer when symptoms were first noticed, because I simply wasn't aware of the disease. Had I checked myself into my primary care provider earlier, I might have been able to catch my cancer at Stage I rather than Stage II, and avoided much of the physical trauma to my body in the process of fighting cancer. And for others, it could mean the difference between life and death! I personally have fought off depression and have had PTSD flashback episodes from my chemotherapy experience that have played back in my head like the trailer for some horror flick, and the same for my RPLND experience. It's not just physical trauma that our bodies experience while going through our treatments, but emotional trauma as well. I certainly could do without such terrible memories of this hell that I've been through.
About the only thing that was more fun than any of this stuff was the Magnesium Citrate that I had to take before the RPLND surgery for "bowel cleansing". It didn't just cleanse my bowels before surgery, but during and for long after as well! It was the gift that kept on giving, but at least the effects were temporary. The havoc wreaked and damage done by the chemotherapy drugs can stick with you forever!
This stuff gave me diarrhea every 2 hours for 36 hours straight, AFTER my RPLND surgery. They thought it was Clostridium difficile aka "C. diff" but nope, just this stuff continuing to work its "magic".
It's by far the most important thing to simply survive cancer and to be a "1" on that spreadsheet as opposed to a "0", and it's certainly important to find the most cost-effective ways of treating and fighting cancer as well in order to extend our limited resources to as many people as possible. But early detection is also important for minimizing impact to quality of life after your fight with cancer and during cancer survivorship. Harsh treatments that weren't needed because a cancer was caught early can't traumatize your body. They can't traumatize your mind. They can't leave you with permanent and lasting side-effects. And they can't rob you of your fertility. If you manage to catch testicular cancer at Stage I and are able to just do surveillance, it doesn't mean that you won't still struggle because I know people who have. We all do in some way. But the less you have to go through to get that cure, the better off you're going to be down the road both physically and mentally. Cancer isn't just about curing the disease, but curing the person and the soul within as well. My cancer fight was a brutal 5 month affair that spanned from February through June 2011, but it wasn't until December of 2013, nearly two and a half years after my treatments ended, until my soul was finally cured of cancer too. As TCAF Founder Kim Jones put it, what comes after your cancer fight really is a "fight for survivorship".
I've made peace with all that my body has been through, and have accepted and know how to manage the various bodily dysfunction and limitations that I have after my caner fight, including having accepted the loss of my fertility. And I've made all of the significant mental adjustments that I've needed to make as far as my approach to life and my attitude as well, but none of this could ever be considered easy. I want the next me and the next you to have a much easier time with this, and spreading awareness about testicular cancer and how to do proper self-exams is exactly the way to go about achieving that. We can't prevent testicular cancer, and what exactly causes it is not even understood yet. So no matter which way you look at things, the earliest possible detection of testicular cancer when it does develop remains the key. It gives you the best possible shot at beating the disease, it minimizes the cost of treatment, and helps to minimize impact to quality of life during survivorship. A testicular self-exam takes less than a minute and is something that should be done at every annual physical, and can and should be done via self-exam once per month. The cost is practically zero. This knowledge and practice is the first line of defense against the most common form of cancer among men aged 15-35, and is hardly something that should be avoided. There's nothing to lose by spreading Awareness about Testicular Cancer and encouraging the practice of Self-Exams. It's a Win-Win-Win.
What I wish had been hanging in my shower in December of 2010, when I first noticed symptoms but ignored them.
StevePake.com